Risk communication in public health is a crucial aspect of managing public health emergencies, outbreaks, and other health-related issues. It involves the exchange of information regarding potential health risks between health authorities, experts, and the public. The World Health Organization defines risk communication as “the real-time exchange of information, advice and opinions between experts or officials and people who face a hazard or threat to their survival, health, or economic or social well-being”
Effective risk communication aims to enhance public understanding of health risks, promote appropriate actions to mitigate those risks, and build trust in health authorities and the information they provide.
On March 12, by popular demand, JGPR Academy will offer its first live class on the topic of risk communication, tailored specifically to public health and emergency management professionals.
Here are some key elements and strategies involved in risk communication in public health:
- Transparency: Openness and transparency are essential in risk communication. This includes providing accurate, timely, and accessible information about the nature of the health risk, its potential consequences, and the actions being taken to address it.
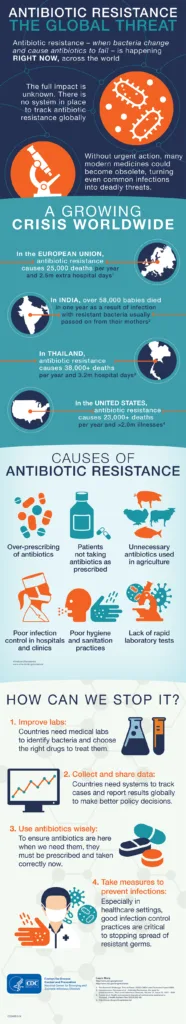
- Clear and Understandable Messaging: Information should be communicated in a clear, understandable manner, avoiding technical jargon or overly complex explanations. Use of visuals, infographics, and plain language can help improve comprehension, especially among diverse audiences.
- Tailored Communication: Recognizing that different audiences have varying levels of health literacy, cultural backgrounds, and information needs, communication strategies should be tailored to address these differences. Messages may need to be adapted for different demographics, such as age groups, language preferences, or socioeconomic status.
- Consistency: Consistent messaging across different channels and among various stakeholders helps to prevent confusion and build trust. Discrepancies or conflicting information can erode public trust and confidence in health authorities.
- Engagement and Participation: Involving the public in the communication process fosters trust and empowers individuals to take appropriate actions to protect their health. This may involve soliciting feedback, addressing concerns, and actively involving community leaders and organizations in disseminating information.
- Empathy and Compassion: Acknowledging and addressing people’s emotions, fears, and concerns with empathy and compassion can help build rapport and trust. Public health communicators should recognize the psychological impact of health threats and offer support and reassurance where needed.
- Proactive Communication: Anticipating and addressing potential questions, uncertainties, or misinformation before they arise can help prevent the spread of rumors and misinformation. Proactive communication also involves providing regular updates and being transparent about any uncertainties or evolving situations.
- Building Trust: Trust is foundational to effective risk communication. Health authorities and communicators must demonstrate credibility, competence, and integrity in their communication efforts. Building trust requires consistency, transparency, empathy, and a commitment to serving the public interest.
- Evaluation and Feedback: Continuous evaluation of communication efforts allows for adjustments and improvements over time. Soliciting feedback from the public, monitoring media coverage, and assessing audience understanding can inform future communication strategies.
- Adaptability: Public health emergencies and health risks are dynamic and evolving situations. Communication strategies should be flexible and adaptable to changing circumstances, new information, and emerging challenges.
Learn about these and more in our live class!
